2. 济宁医学院附属济宁市第一人民医院, 济宁 272011
2. Jining NO.1 People's Hospital & the Affiliated Hospital of Jining Medical University, Jining 272011, China
动脉粥样硬化性心脑血管疾病是全世界人类死亡的最常见原因, 其中血脂异常,特别是血清胆固醇水平升高被认为是导致血管粥样硬化的最重要因素[1]。在生理上,雌激素可以维持高水平的高密度脂蛋白胆固醇(HDL-C)和低水平的低密度脂蛋白胆固醇(LDL-C)和甘油三酯(TG)[2]。对于围绝经期女性而言,激素变化和月经的暂停可以显著改变女性的血脂水平[3],与心脑血管疾病发生密切相关[3-4]。目前有关血脂与冠心病发病关系的研究国内外已有不少文献报道,但对于围绝经期女性这个特殊人群的血脂谱研究较少。本研究目的在于探讨非高密度脂蛋白(non-HDL-C)水平在围绝经期女性冠脉病变严重程度中的临床意义。
1 资料和方法 1.1 一般资料收集2017年8月至2019年5月于济宁市第一人民医院心内科住院行冠脉造影术并确诊为冠心病的40~60岁围绝经期女性患者,选取符合纳入及排除标准的患者69例,按Gensini积分分为两组:轻中度冠脉病变组(n=42,GS<50)和重度冠脉病变组(n=27,GS≥50)。本研究通过济宁医学院附属济宁市第一人民医院伦理委员会审核并批准,所有入选患者均签署知情同意书。纳入标准:1)年龄40~60岁女性,平均年龄50岁,其中围绝经期以出现月经紊乱至停经1年内为标准;2)符合以下冠心病诊断标准:将左主干(LM)、前降支(LAD)、回旋支(LCX)和右冠状动脉(RCA)定义为主要冠状动脉,任何一支主要冠状动脉直径狭窄≥50%,其中左主干(LM)狭窄≥40%为阳性;3)所有患者入院前均未服用降血脂药物。排除标准:1)由于长期月经失调、疾病、手术或药物所致的月经紊乱或停经者;2)近期有急性、慢性感染性疾病和糖尿病、甲状腺、恶性肿瘤、肝、肾功能不全等疾病;3)既往行冠状动脉支架植入术(PCI)及冠状动脉旁路移植术(CABG);4)未签署知情同意书的人群。
1.2 方法1) 记录患者入院时一般资料。资料包括年龄、体重指数(BMI)、吸烟史、饮酒史,高血压病史、糖尿病病史、脑梗死病史。入院后行冠脉造影术前完善血常规、肝功、肾功(包括尿酸、肌酐、β2微球蛋白)、血糖、血脂(包括总胆固醇、甘油三酯、低密度脂蛋白胆固醇、极低密度脂蛋白胆固醇、高密度脂蛋白胆固醇、非高密度脂蛋白、载脂蛋白A1、载脂蛋白B、脂蛋白)、电解质、B型钠尿肽前体、心肌酶谱、术前免疫及心电图、心脏彩超等检查。2)冠脉造影检查。入选的所有患者行冠脉造影采用Judkins法常规体位投照,取多部位造影,通常左冠脉取6个投照体位,右冠取3个体位,术后冠脉造影结果由两名有经验的介入医师进行判断并详细记录冠脉病变部位及狭窄程度。3)冠脉病变界定。冠状动脉病变支数的界定:以冠状动脉左主干或心外膜下3条主要冠状动脉前降支(LAD)、回旋支(LCX)、右冠状动脉(RCA)及大分支其任何一段直径狭窄≥50%即为病变有意义。4)Gensini积分评定。冠状动脉病变严重程度评判采用Gensini积分方法[5]。
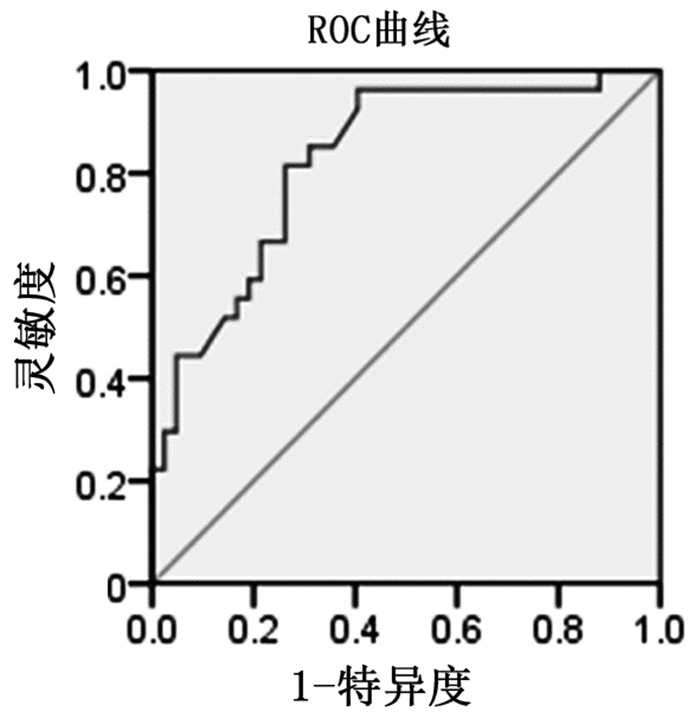
1.3 统计学方法所有数据均采用SPSS 22.0统计学软件进行处理、分析,其中计量资料(符合正态分布)以表示,两组间比较采用两独立样本t检验;计数资料用百分构成比表示,组间比较采用χ2检验。多因素分析采用二元logistic回归分析,将单因素分析中P<0.05的变量纳入多因素logistic回归分析。以受试者工作特性(ROC)曲线来评价non-HDL-C水平对冠脉病变程度的诊断价值。其检验水准为α=0.05(双侧检验)。
2 结果 2.1 两组患者一般临床指标的比较轻中度冠脉病变组高血压病比例高于重度冠脉病变组,重度冠脉病变组中TC、TG、LDL-C、non-HDL-C、apOB及Gensini Score水平均高于轻中度冠脉病变组(P<0.05)。见表 1。
| 表 1 不同严重程度冠脉病变患者临床指标的比较 |
将表 2中具有统计学差异的指标及年龄纳入二元logistic回归多因素分析,以P<0.05为具有统计学意义。围绝经期女性患者的non-HDL-C水平可作为评估冠脉病变严重程度的独立危险因素(OR=4.223,P<0.01,95%CI:1.516~11.765);该类患者LDL-C水平亦可作为评估冠脉病变严重程度的独立危险因素(OR=5.390,P<0.01,95%CI:1.557~18.653)。见表 2。
| 表 2 二元logistic回归多因素分析 |
针对Gensini Score绘制ROC曲线。曲线下面积为0.874(95%CI:0.794~0.955,P<0.001);最佳切点为3.36mmol/L,对应灵敏度为96.3%,特异度为66.7%。即non-HDL-C>3.36mmol/L,则认为该患者存在严重冠脉病变的风险。见图 1。
|
图 1 non-HDL-C与Gensini Score间ROC曲线 |
流行病学研究显示,社会老龄化趋势逐年升高,围绝经期女性的数量也迅速增长。而心血管疾病并没有引起绝大多数围绝经期女性的高度关注与重视,由于更年期与女性心血管疾病发病时间接近,而且围绝经期女性缺乏典型的临床症状,容易被患者及临床医生所忽视。因此因更年期综合征而就诊的女性均应常规作心血管疾病高危因素的筛查,要关注并重视对广大围绝经期女性血脂水平的检测,为更好地预测心血管疾病风险,进一步为女性心血管相关疾病的治疗和预防提供临床依据。
多年来,LDL-C被认为是心血管疾病危险因素和脂质标志物之一,在动脉粥样硬化性心血管疾病(ASCVD)的发生、发展中起重要作用[6]。LDL-C也被认为是指导脂质管理的主要标志物[7]。然而,有证据质疑LDL在ASCVD发展中的地位[8],随着研究的不断深入,近年来有学者建议以non-HDL-C作为血脂治疗的主要目标,特别是对于高甘油三酯血症或心脏代谢异常的患者[9-10]。大量Meta分析及前瞻性研究比较了LDL和non-HDL-C在心血管风险预测中的作用[11-12],结果显示,在与心血管风险相关性方面,apoB和non-HDL-C可能优于LDL-C[13],最可能的原因是每个致动脉硬化脂蛋白的颗粒,如LDL、VLDL和脂蛋白(a)携带一个apoB分子,因此血浆apoB的浓度可以反映致动脉粥样硬化潜能的总和。同时,non-HDL-C的组分都是具有潜在致动脉粥样硬化的含apoB的脂蛋白颗粒的胆固醇[14]。此外,一些临床和遗传学研究认为富含TG的脂蛋白胆固醇水平(残余胆固醇)是缺血性心脏病的确定病因[14]。另一个可能的原因与LDL颗粒有关,Zhu等[15]研究表明,与LDL-C相比,non-HDL-C与致动脉粥样硬化脂蛋白亚组分(小LDL亚组分)更具正相关性,同时与抗动脉粥样硬化脂蛋白亚组分(大HDL亚组分)更具负相关性。因此,与LDL-C相比,apoB和non-HDL-C可以更准确地反映LDL颗粒的特征。
相关Meta分析显示[16],non-HDL-C水平与冠脉病变密切相关(RR=1.79,95%CI:1.68~1.91)。此外,常程等[17]研究共纳入132例青年冠心病患者,根据Gensini评分将分为轻中度冠脉病变组(GS 1-59,n=78)及重度冠脉病变组(GS≥60,n=54),进行二元logistic分析non-HDL-C可作为预测冠脉病变严重程度的独立危险因素(OR=1.061,P=0.041,95%CI:1.002~1.123),ROC曲线分析示non-HDL-C>3.58mmol/L,可预测出现冠状动脉严重病变。本研究发现围绝经期女性冠心病患者的non-HDL-C水平可作为评估冠脉病变严重程度的独立危险因素(OR=4.223,P<0.001,95%CI:1.516~11.765),通过ROC曲线对non-HDL-C水平预测冠脉病变严重程度进行分析,得到最佳切点为3.36mmol/L,其灵敏度为96.3%,特异性为66.7%,这与上述观点相符。这表明,non-HDL-C可以更好地反映围绝经期女性冠心病患者发病情况及冠脉病变严重程度,为今后临床工作中开展早期血脂筛查、血脂异常诊断和治疗,预防或延缓围绝经期女性心血管疾病提供参考依据。
| [1] |
Jellinger PS. American association of clinical Endocrinologists/American college of Endocrinology management of dyslipidemia and prevention of cardiovascular disease clinical practice guidelines[J]. Diabetes Spectr, 2018, 31(3): 234-245. DOI:10.2337/ds18-0009 |
| [2] |
Pardhe BD, Ghimire S, Shakya J, et al. Elevated cardiovascular risks among postmenopausal women:a community based case control study from nepal[J]. Biochem Res Int, 2017, 2017: 3824903. DOI:10.1155/2017/3824903 |
| [3] |
Zhang J, Wang H, Yang S, et al. Comparison of lipid profiles and inflammation in pre-and post-menopausal women with cerebral infarction and the role of atorvastatin in such populations[J]. Lipids Health Dis, 2018, 17(1): 20. DOI:10.1186/s12944-018-0669-9 |
| [4] |
Reddy KS, Chandala SR. A comparative study of lipid profile and oestradiol in pre-and post-menopausal women[J]. J Clin Diagn Res, 2013, 7(8): 1596-1598. DOI:10.7860/JCDR/2013/6162.3234 |
| [5] |
Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease[J]. Am J Cardiol, 1983, 51(3): 606. DOI:10.1016/s0002-9149(83)80105-2 |
| [6] |
Reiner Z, Catapano AL, De Backer G, et al. ESC/EAS Guidelines for the management of dyslipidaemias:the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS)[J]. Eur Heart J, 2011, 32(14): 1769-1818. DOI:10.1093/eurheartj/ehr158 |
| [7] |
Ray KK, Kastelein JJ, Boekholdt SM, et al. The ACC/AHA 2013 guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults:the good the bad and the uncertain:a comparison with ESC/EAS guidelines for the management of dyslipidaemias 2011[J]. Eur Heart J, 2014, 35(15): 960-968. DOI:10.1093/eurheartj/ehu107 |
| [8] |
DuBroff R. Cholesterol paradox:a correlate does not a surrogate make[J]. Evid Based Med, 2017, 22(1): 15-19. DOI:10.1136/ebmed-2016-110602 |
| [9] |
An International Atherosclerosis Society Position Paper: global recommendations for the management of dyslipidemia--full report[J].J Clin Lipidol, 2014, 8(1): 29-60.DOI: 10.1016/j.jacl.2013.12.005. http://www.sciencedirect.com/science/article/pii/S0021915013006813
|
| [10] |
Jacobson TA, Ito MK, Maki KC, et al. National lipid association recommendations for patient-centered management of dyslipidemia:part 1--full report[J]. J Clin Lipidol, 2015, 9(2): 129-169. DOI:10.1016/j.jacl.2015.02.003 |
| [11] |
Boekholdt SM, Arsenault BJ, Mora S, et al. Association of LDL cholesterol, non-HDL cholesterol, and apolipoprotein B levels with risk of cardiovascular events among patients treated with statins:a meta-analysis[J]. JAMA, 2012, 307(12): 1302-1309. DOI:10.1001/jama.2012.366 |
| [12] |
Di AE, Gao P, Pennells L, et al. Lipid-related markers and cardiovascular disease prediction[J]. JAMA, 2012, 307(23): 2499-2506. DOI:10.1001/jama.2012.6571 |
| [13] |
Zhang Y, Wu NQ, Li S, et al. Non-HDL-C is a better predictor for the severity of coronary atherosclerosis compared with LDL-C[J]. Heart Lung Circ, 2016, 25(10): 975-981. DOI:10.1016/j.hlc.2016.04.025 |
| [14] |
Varbo A, Benn M, Tybjærg-Hansen A, et al. Remnant cholesterol as a causal risk factor for ischemic heart disease[J]. J Am Coll Cardiol, 2013, 61(4): 427-436. DOI:10.1016/j.jacc.2012.08.1026 |
| [15] |
Zhu CG, Zhang Y, Xu RX, et al. Circulating non-HDL-C levels were more relevant to atherogenic lipoprotein subfractions compared with LDL-C in patients with stable coronary artery disease[J]. J Clin Lipidol, 2015, 9(6): 794-800. DOI:10.1016/j.jacl.2015.08.010 |
| [16] |
Liu H, Deng X, Peng Y, et al. Meta-analysis of serum non-high-density lipoprotein cholesterol and risk of coronary heart disease in the general population[J]. Clin Chim Acta, 2017, 471: 23-28. DOI:10.1016/j.cca.2017.05.006 |
| [17] |
常程, 潘一龙, 李晓东. 非高密度脂蛋白胆固醇水平与青年冠心病的相关性[J]. 中国循证心血管医学杂志, 2018, 10(8): 952-956. DOI:10.3969/j.issn.1674-4055.2018.08.16 |